Creating fabric was traditionally done by conversion of fibers into yarns and yarns into fabrics either by weaving or knitting. Then came the introduction of nonwovens in the 19th century. In 1962, the first written definition of nonwovens was initiated by American Society for Testing and materials which defined the term as “textile fabrics made of carded web or fiber web held together by adhesives”.
Nonwoven materials became an especially vital section of the textile trade in recent years. The technical developments in polymers, nonwoven process and cloth finishing have crystal rectifier to important enhancements in cloth physical and mechanical properties as well as cloth handling and drapability, tensile properties, abrasion resistance, pilling and laundry stability, colouring and printing that make prospects for nonwoven cloth applications particularly in attire clothing.
Test method applicable to nonwovens
https://ipstesting.com/industries-served/nonwovens/nonwovens-testing/
| Title | Method Number |
| Test Methods for nonwovens – Part 6: Absorption | ISO 9073-6 |
| Colorfastness to Crocking: Crockmeter Method | AATCC 8 |
| Taber Abrasion | TAPPI T 476 |
| Fiber Analysis of paper and paper board | TAPPI T 401 |
| Water Resistance: Impact Penetration Test | AATCC 42 |
| Water Resistance: Hydrostatic Pressure Test | AATCC 127 |
| Gray Scale for Staining | AATCC EP 2 |
| Air Permeability of Textile Fabrics | ASTM D 737 |
| Failure in Sewn Seams of Woven Apparel Fabrics | ASTM D 1683 |
| Propagation Tear Resistance of Plastic Film and Thin Sheeting by Pendulum Method | ASTM D 1922 |
| Mass Per Unit Area (Weight) of Fabric | ASTM D 3776 |
| Bursting Strength of Textile Fabrics – Diaphragm Bursting Strength Tester Method | ASTM D 3786 |
| Breaking Strength and Elongation of Textile Fabrics (Grab Test) | ASTM D 5034 |
| Breaking Force and Elongation of Textile Fabrics (Strip Method) | ASTM D 5035 |
| Tearing Strength of Nonwoven Fabrics by the Trapezoid Procedure | ASTM D 5733 |
| Bursting Strength of Fabrics Constant Rate of Extension (CRE) Ball Burst Test | ASTM D 6797 |
| Test methods for Nonwovens – Part 10: Lint and other particles generation in the dry state. | ISO 9073-10 |
| Tearing Strength of Fabrics by Falling-Pendulum (Elmendorf-Type) Apparatus | ASTM D1424 |
| Impact Resistance of Plastic Film by the Free-Falling Dart | ASTM D1709 |
| Bursting Strength of Textiles – Constant-Rate-of-Traverse (CRT) Ball Burst Test | ASTM D3787 |
| Abrasion Resistance of Textile Fabrics (Rotary Platform, Double-Head Method) | ASTM D3884 |
| Total Energy Impact of Plastic Films by Dart Drop | ASTM D4272 |
| Tearing Strength of Fabric by Trapezoid Procedure | ASTM D5587 |
| Standard practice for Calculating Yellowness and Whiteness Indices from Instrumentally Measured Color Coordinates | ASTM E313 |
| Laboratory Test Method for 16 CFR Part 1610: Standard for Flammability of Clothing Textiles Laboratory Test Manual | CFR 1610 |
| Absorption, Time and Rewet – Single Insult (Specimen cut from Whole Product) | IPS Method |
| Absorption, Time – Liquid Strike-Through, Repeated (Specimen cut from Whole Product) | IPS Method |
| Absorption, Time – Liquid Strike-Through (Specimen cut from Whole Product) | IPS Method |
| Absorption, Capacity – 4″ x 4″ Specimen (Tissue and Thin Absorbent Products) | IPS Method |
| Absorption, Time and Rewet – Three Insults (Specimen cut from Whole Product) | IPS Method |
| Title | Method Number |
| Textile Test Methods – Textile Fabrics – Determination of Resistance to Water Penetration – Hydrostatic Pressure Test | ISO 811:1981 |
| Textiles – Test methods for nonwovens – Part 3: Determination of tensile strength and elongation | ISO 9073-3 |
| Textiles – Determination of the Permeability of Fabrics to Air | ISO 9237 |
| Water vapor transmission rate of paper and paperboard at 23 °C. and 50% RH | TAPPI T 448 |
| Water vapor transmission rate of paper and paperboard at high temperature and humidity. | TAPPI T 464 |
| Absorption, Time – Wet Out (Tissues and Nonwovens ) | US Patent 7166189 |
| Three Standard Test Methods for Nonwoven Absorption | WSP 10.1 |
| Evaluation of Oil and Fatty Liquids Absorption | WSP 10.4 |
| Abrasion Resistance of Nonwoven Fabrics Using a Nonwoven Modified Martindale Abrasion Test Method | WSP 20.5 |
| Electro Static Decay of Nonwoven Fabrics | WSP 40.2 |
| Air Permeability of Nonwoven Materials | WSP 70.1 |
| Nonwoven Coverstock Liquid Strike-Through Time Using Simulated Urine. | WSP 70.3 |
| Wetback After Repeated Strike-Through Time | WSP 70.8 |
| Rate of Acqusition and Re-Wet | WSP 70.9 |
| Centrifugal Liquid Retention Capacity | WSP 70.10 |
| Evaluation of Water Penetration (Spray Impact Test) of Nonwoven Fabrics. | WSP 80.3 |
| Evaluation of Water Resistance (Hydrostatic Pressure) Test | WSP 80.6 |
| Nonwovens Coverstock Wetback | WSP 80.10 |
| Stiffness of Nonwoven Fabrics Using the Cantilever Test | WSP 90.1 |
| Tearing Strength of Nonwoven Fabrics by Falling-Pendulum (Elmendorf) Apparatus. | WSP 100.1 |
| Testing Strength of Nonwoven Fabrics by the Trapezoid Procedure | WSP 100.2 |
| Breaking Strength and Elongation of Nonwoven Materials (Grab Strength Test) | WSP 110.1 |
| Standard Test Method for Breaking Force and Elongation of Nonwoven Materials (Strip Method) | WSP 110.4 |
| Resistance to Mechanical Penetration (Ball Burst Procedure) of Nonwoven Fabrics | WSP 110.5 |
| Mass per Unit Area. | WSP 130.1 |
| Resistance to Linting of Nonwoven Fabrics | WSP 160.1 |
| Cup Crush | WSP 402.0 |
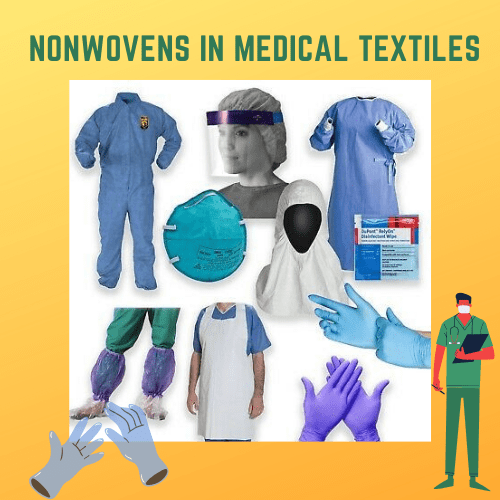
Nonwovens in medical textiles
The use of nonwovens in medical field goes back to the time of Second world war when the need was enormous for production of medical products. In many reports printed, nonwovens were considered the foremost effective materials for microorganism barriers. They were conjointly found superior to linens within the reduction of air-borne contamination.
After important development of nonwovens, they were designed in a very thanks to suit the medical wants and provides a performance far better than their woven counterparts in terms of price, effectiveness, disposability etc. In hospitals, cross-contamination is usually one among the most important issues that were attributed mostly to re-using of woven robes, masks and alternative similar articles which might get contaminated and doubtless unfold the germs.
Material used in medical nonwovens:
The fibers used in medical nonwovens can be classified in natural and synthetic categories. The natural fibers used are wood-pulp, cotton and rayon. Wood pulp is used for its obvious absorbency, bulk and low cost. Cotton and rayon are good to be used directly on wounds. They have good absorbency and make excellent nonwovens.
The reasons natural fibers make excellent medical nonwovens are:
They are highly absorbent of exudate and blood
Excellent breathability
Good aesthetic characteristics
Easy launderability and can be sterilized
Excellent dimensional stability and high operability temperature ~ 175 deg C
Biodegradable
Excellent drape and conformability
Good heat resistance
Excellent water retaining capacity
Nonallergenic and non-irritant fibers
The synthetic fibers mostly used in this application are: polypropylene for its excellent rheological characteristics, hydrophobicity which is desired in some systems where barrier properties are required, low cost, bicomponent fibers which are widely used in thermal bonding and added functionality and polyester when strength, mechanical properties and ease of sterilization are of prime importance. Synthetic fibers also account for the products strength, solvent resistance, static dissipation and many other desirable properties.
The properties of synthetic fibers which are required in many applications:
Hydrophobicity: to be able to act as a barrier fabric
Easy to process
Cost effectiveness
Better performance due to strength, low density
Easy to dispose, not hazardous
https://www.technicaltextile.net/articles/nonwovens-as-medical-textiles-3693
Felted Fabrics
Wool felt is the most common non-woven fabric and is produced by using short staple fibres from wool or other animal hairs (such as camel). Wool is an ideal fibre because its surface has natural hooks like scales, which when moisture, heat and vigorous movement are applied, interlock with each other. The heat and damp conditions cause the fibres to curl up, and the scales locking together prevents the fibres from straightening out again. When you wash a natural wool jumper and it shrinks in size the jumper is actually felting and you can’t make it bigger again no matter how hard you try to stretch it back.
Bonded Fabrics
There are three main methods of making bonded fabrics:
- Dry laid: a web of fibres is laid in a drum and hot air is injected to bond the fibres together.
- Wet-laid: a web of fibres is mixed with a solvent that softens the fibres and releases a glue-like substance that bonds the fibres together and then the web is laid out to dry.
- Direct spun: the fibres are spun on to a conveyer belt and glues are sprayed on to the fibres, which are then pressed to bond; if the fibres are thermoplastic (will change shape with heat) then the glue is not needed in this process.
Felted and bonded fabrics applications
Hats, jackets, toys and snooker table covers are some commonly used for wool felts.
Bonded fabrics are used for disposable products such as cloths, medical masks, and table linen. They are also used for interfacings for stiffening and strengthening clothing and dressmaking (e.g. Vilene).
Laminated Fabrics
Laminated fabrics are made by bonding two or more fabrics together. Many fabrics require extra insulation or protection, and the foam is bonded to provide this. Sometimes comfort can be an issue with PVC fabrics, so a softer fabric may be bonded instead of using a lining. Making a fabric breathable and waterproof may require lamination of a membrane, as in Gortex and Sympatex.
https://www.textileschool.com/352/non-woven-fabrics/
LIST OF NON WOVEN MANUFACTURING COMPANIES IN INDIA
B M TRADERS – NON WOVEN INTERLINING
http://nonwoveninterlining.com/
TEXONFABRICS
https://www.texonfabrics.com/PP%20Non-Woven%20Fabric%20Rolls.html
ADITYA NONWOVEN FABRIC PVT LTD
http://www.adityanonwovenfabric.com/
SIDWIN NON WOVEN FABRICS
KT EXPORTS INDIA
MARUTI POLYFABS
SURYA TEXTECH
DATA
Exporters
This treemap shows the share of countries that export Non-woven Textiles.

Importers
This treemap shows the share of countries that import Non-woven Textiles.

https://oec.world/en/profile/hs92/5603/
NON-WOVEN MATERIALS IN MEDICAL TEXTILES
Facemasks
How are Masks Made?
face masks are made with non-woven fabric, which has better bacteria filtration and air permeability while remaining less slippery than woven cloth. The material most commonly used to make them is polypropylene, either 20 or 25 grams per square meter (gsm) in density. Masks can also be made of polystyrene, polycarbonate, polyethylene, or polyester.
20 gsm mask material is made in a spunbond process, which involves extruding the melted plastic onto a conveyor. The material is extruded in a web, in which strands bond with each other as they cool. 25 gsm fabric is made through meltblown technology, which is a similar process where plastic is extruded through a dye with hundreds of small nozzles and blown by hot air to become tiny fibers, again cooling and binding on a conveyor. These fibers are less than a micron in diameter.
Surgical masks are made up of a multi-layered structure, generally by covering a layer of textile with non-woven bonded fabric on both sides. Non-wovens, which are cheaper to make and cleaner thanks to their disposable nature, are made with three or four layers. These disposable masks are often made with two filter layers effective at filtering out particles such as bacteria above 1 micron. The filtration level of a mask, however, depends on the fiber, the way it’s manufactured, the web’s structure, and the fiber’s cross-sectional shape. Masks are made on a machine line that assembles the nonwovens from bobbins, ultrasonically welds the layers together, and stamps the masks with nose strips, ear loops, and other pieces.
Completed masks are then sterilized before being sent out of the factory.
Surgical Mask Tests
Once surgical masks are made, they must be tested to ensure their safety in various situations. There are five tests they must be put through:
- Bacteria filtration efficiency in vitro (BFE). This test works by shooting an aerosol with staphylococcus aureus bacteria at the mask at 28.3 liters per minute. This ensures the mask can catch the percentage of bacteria it’s supposed to.
- Particle Filtration Efficiency. Also known as the latex particle challenge, this test involves spraying an aerosol of polystyrene microspheres to ensure the mask can filter the size of the particle it’s supposed to.
- Breathing resistance. To ensure the mask will hold its shape and have proper ventilation while the wearer breathes, breathing resistance is tested by shooting a flow of air at it, then measuring the difference in air pressure on both sides of the mask.
- Splash resistance. In splash resistance tests, surgical masks are splashed with simulated blood using forces similar to human blood pressure to ensure the liquid cannot penetrate and contaminate the wearer.
- Flammability. Since several elements of an operating room can easily cause fire, surgical masks are tested for flammability by being set on fire to measure how slowly it catches and how long the material takes to burn. ASTM levels 1, 2, and 3 are all required to be Class 1 flame resistant.
https://www.thomasnet.com/articles/other/how-surgical-masks-are-made/
- Surgical Disposable Non Woven Masks Medical 3ply Disposable Face Masks for Covid-19

- Anti-pollution N95 Face Mask with Breathing Valve and Ear Loops

https://www.seniority.in/anti-pollution-n95-face-mask-with-breathing-valve-and-ear-loops-san-nap-pdp
- 3M mask

https://www.tinkleo.com/goods/masks/11291.html
PPE kit for Covid19
Personal Protective Equipments (PPEs) are protective gears designed to safeguard the health of workers by minimizing the exposure to a biological agent.
Components of PPE are goggles, face-shield, mask, gloves, coverall/gowns (with or without aprons), head cover and shoe cover.
https://www.mohfw.gov.in/pdf/GuidelinesonrationaluseofPersonalProtectiveEquipment.pdf

CDC Recommendations
The U.S. Centers for Disease Control recommend certain guidelines for healthcare workers who will come into contact with the virus. Workers should use several types of PPE if available to keep from getting infected:
Gowns. ANSI or AAMI PB70 Level 3 or 4 isolation gowns are recommended for medium to high risk of contamination where a large critical zone is needed. Surgical gowns at levels 1-4 can be worn for all levels of exposure while in surgery, and ANSI/AAMI PB70 Level 1 or 2 gowns can be worn for activities with minimal risk of exposure. Gowns should cover the wearer’s back even when they bend over or sit.
Coveralls. Coveralls can be worn in place of gowns. They provide better protection, but they also are more uncomfortable to most healthcare workers thanks to the added insulation. Additionally, healthcare workers are often more unfamiliar with coveralls, which can lead to risks if coveralls aren’t properly removed.
Gloves. Nonsterile patient examination gloves can be used to treat coronavirus patients. These can include nitrile, natural, rubber, polychloroprene, and vinyl gloves. Double gloving and extended length gloves are not considered necessary.
Respirators. Surgical N95 respirators, which can filter out bacteria and viruses, should only be worn by healthcare workers in sterile environments or who are at risk of airborne or fluid hazards such as sprays. Nonsurgical N95s can be worn by healthcare workers outside of surgery who are in contact with coronavirus patients. If no respirators are available, workers are advised to wear the next best level of protection, such as a face mask.
Eye protection. This can be a face shield or goggles. Reusable goggles and shields should be cleaned and disinfected after every use, and disposable types should be thrown out after every use. This should be removed before leaving the patient care area.
https://www.thomasnet.com/articles/plant-facility-equipment/how-to-make-ppe/

Indian actor Shahruk Khan volunteers to provide 25,000 PPE kits for healthcare workers in Maharashtra.
Indian Actress Kangana Ranaut contributes 25 lakh for covid19 relief

Actress Madhuri Dixit and her husband Dr Shriram Nene have pledged to donate to the PM CARES Fund and CM’s Relief Fund to fight the coronavirus pandemic (COVID-19).

With the news in all doom and gloom its not always possible to keep our self-positive but let’s be optimistic and have hope in the advances of medical textile that will surely help to overcome the pandemic in the time to come. This pandemic will also create awareness of how important nonwovens are in textile industry.
The article was written by – Ms. Ayman Satopay. B.Sc in Textile and Apparel Design from Sir Vithaldas Thackersey College Of Home Science. Textile Value Chain trainee editor. Email: tvcmedia.digital@gmail.com